Cannabis-based products for medical use in humans

Project Optimus
Pharmacokinetics in dermatology drug development
Topical medications are applied to the skin or eyes to achieve a specific local therapeutic effect. However, delivering these medications is challenging due to the skin’s effective barrier properties. Unlike orally or intravenously administered drugs, topicals require different pharmacokinetic (PK) assessments. Many studies for topicals are postponed until the final formulation, strength, and dosing regimen are confirmed through safety and efficacy trials. Nonetheless, early sampling for systemic exposure is recommended to verify assay sensitivity, safety coverage, optimal dosing regimen, and sampling. Various drugs fall into the category of topical medications, such as:
- Lotions, creams, and ointments
- Gels
- Foams
- Patches
- Liquid drops
- And others
Drug Absorption Through the Skin Barrier
Topical drugs are applied directly to the skin, targeting it as the main site of action. Ideally, these drugs should not penetrate deeply enough to enter the bloodstream, as systemic absorption can pose safety risks. The skin is made up of multiple layers that protect against harmful substances and microbes, with the stratum corneum being the primary barrier. Traditionally, it was thought that topical drugs did not significantly penetrate the skin’s barrier, but this is not always the case. Corticosteroids are a prime example of drugs that can be absorbed through the skin, potentially leading to systemic side effects like cortisol suppression. The penetration of topical drugs depends on various factors, including the drug’s chemical properties and the condition of the skin. The ingredients in the drug formulation can also impact absorption, with penetration enhancers like ethanol or propylene glycol helping other substances reach deeper skin layers.
Development Challenges for Topically Applied Drugs
Developing topically applied drugs presents numerous challenges for developers. These formulations must deliver the correct amount of medication to the target area, maintain physical and chemical stability, and be cosmetically pleasing without causing skin irritation. Significant changes to a formulation during development often necessitate repeating studies. Since systemic exposure can be minimal with topical applications, characterizing the pharmacokinetic (PK) profile demands a sensitive bioanalytical assay.
Regulatory Questions for Topical Drug Development
Over the past two decades, regulatory agencies have begun requiring drug developers to address two critical questions outlined in the FDA’s guidance on maximal usage trials for topically applied drugs. By answering these questions, agencies can assess drug safety and determine appropriate labelling and clinical use recommendations, such as the necessity for further safety evaluations and dosing considerations for special populations.
- When the drug is applied to the skin, does it penetrate the skin barrier and cause measurable systemic exposure?
- If so, what is the extent of systemic exposure to the active ingredient?
Maximal Usage Trial Design for Topical Drugs
A common PK trial design for topically applied drugs is the Maximal Usage Trial (MUsT). MUsTs aim to maximize drug exposure to understand systemic absorption and exposure at clinically relevant doses, typically within the most severely affected patient group. These trials are crucial because this information may not be captured in Phase 2 or Phase 3 studies, where moderate doses are more commonly used. The FDA has issued guidance for maximal usage trials for over-the-counter products, but the principles apply to all topical products. Systemic exposure is evaluated through PK analysis, providing insights into absorption, distribution, and elimination from the body. This analysis also determines exposure estimates and key PK parameters such as:
- Maximum blood or plasma concentration (Cmax)
- Time of maximum concentration (Tmax)
- Area under the concentration-time curve (AUC)
- Elimination rate (half-life)
Unique Considerations in Dermal Maximal Usage Trials
- Frequency and Duration of Dosing: The dosing frequency and duration should maximize drug absorption and align with the proposed labeling and anticipated use, using the maximum proposed drug strength.
- Body Surface Area (BSA): Topical drugs may be applied over varying BSAs, from small areas to nearly the entire skin surface (e.g., sunscreen). Higher BSA coverage can lead to increased systemic absorption, so the BSA in MUsT should reflect anticipated clinical use.
- Bioanalytical Methods: Validated and sensitive bioanalytical methods are essential for both active ingredients and key metabolites, given their role in PK assessments for dosing and labeling.
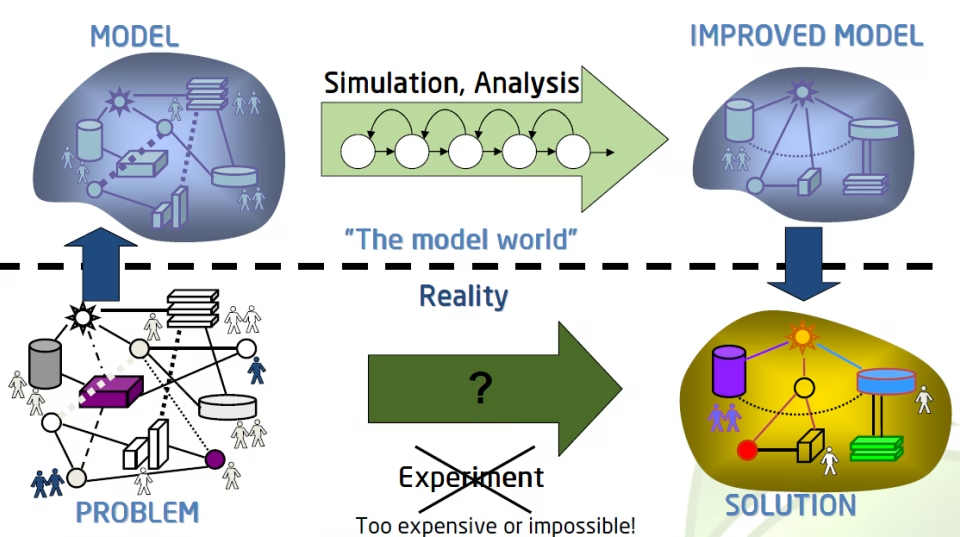
- Population Pharmacokinetics (popPK): PopPK modeling can identify parameters and covariates such as age, disease severity, BSA of application, and concomitant medications influencing exposure. Studies involving healthy volunteers may not be informative for PK due to differing skin barrier properties compared to the intended patient population.
PK Parameters & Sampling Schedules in MUsTs
The goal of MUsT is to determine exposure parameters and assess systemic absorption. Blood sampling schedules should be designed to derive key parameters like Cmax, Tmax, AUC0-last, AUC0-inf, and AUCtau (if repeated doses are administered). Multiple absorption phases and elimination rates, which can be slow and limited by absorption, complicate PK analysis. Sampling adjustments may be necessary for specific populations, such as pediatric studies. Sampling should align with the expected concentration versus time profile of the drug. Generally, sampling following multiple dosing is required, especially when the condition improves with treatment.
Other Considerations for Topical Drug Development
Several factors external to the drug product can impact systemic exposure for topically applied medications, including:
- Self-Application: Patients may believe that using more product leads to faster healing. Loose dosing terminology (e.g., “pea-sized”) may require subject training and observation during MUsT studies to control drug quantity variability.
- Occlusion: The application site can affect drug absorption. Occlusion, whether intentional (e.g., occlusive patches) or inadvertent (e.g., clothing), can enhance penetration and systemic exposure. Understanding if occlusion increases systemic absorption is important for product labeling.
- Skin Defects: The skin’s barrier function can be compromised by abrasions, soaps, antiseptics, or the removal of natural oils, potentially leading to increased drug absorption. These factors should be considered in MUsT study design.
Conclusions
PK studies are necessary for topical drugs, even if systemic exposure is thought to be minimal or nonquantifiable. The complexity of topical drugs requires careful design and analysis of these studies. When designing MUsT trials, consider the properties of the drug components and expected use conditions. Clinical pharmacology input is crucial to optimize study designs, PK sampling, and assess potential safety risks based on systemic exposure. A well-developed clinical pharmacology plan is essential for any new topical drug product. Thaison Consulting has extensive expertise in pharmaceutical dermatology drug development. Contact our experienced clinical pharmacologists and pharmacokineticists to discuss strategy, design, PK sampling schedules, noncompartmental PK analysis, and population PK for your topical medication.