
Pharmacokinetics in dermatology drug development
10 Reasons to Implement Modelling and Simulations Into Your Drug Development Program
What is Project Optimus?
In 2016, the United States passed the 21st century Cure Act and along with that came the Cancer Moonshot initiative, which had the goal to reduce death rates from cancer by greater than 50% over the next 25 years. To accomplish this, the FDA established the oncology center of excellence, along with nearly $2 billion in funding to accelerate scientific discovery, foster greater collaboration, and improve sharing of cancer data. Since then, the Cancer Moonshot program has facilitated over 300 initiatives, ranging on panel discussion to research grants, and of course, Project Optimus.
Historically, many oncology therapeutics were highly cytotoxic with the idea that they had a linear dose response. Therefore, as the dose increased, we would expect that they would have better tumour responses and better efficacy leading to the maximum tolerated doses being selected for further drug development and eventual approval.
However, patient populations in the real world had worse conditions, had more comorbidities, worse performance score and they often were not able to tolerate high dosages for as long as they were intended, having to stop therapy soon after starting due to adverse event. Physicians were also voicing their concerns due to the lack of data supporting dose adjustments for these patients. Consequently, when adverse events occurred, they were uncertain whether to lower the dose, temporarily pause the treatment, or discontinue the therapy entirely.
Project Optimus is intended to reform the dose optimisation and dose selection paradigm in oncology drug development. Dose optimisation is looking at efficacy, toxicity and long-term safety data, and determining which dose level or dose regimen has the best benefit to risk ratio.
Which sponsors are affected by Project Optimus?
This applies to all sponsors, whether you have a cytotoxic therapy or a targeted therapy, anyone in early phase clinical research really needs to be aware of these new requirements and follow them as their the new expectations from the FDA. This will ensure optimal treatment and dose regiments for patients, improve overall outcomes and allow physicians to have a better idea of how to manage their therapies as these new drugs are being developed.
What must development programs do differently to gain regulatory acceptance of their recommended Phase 2 dose?
Sponsors are required to analyse all the available safety data, including dose limiting toxicities, serious adverse events, all the treatment emergent adverse events, the preliminary efficacy data, as well as PKPD, dose/exposure-response analysis, which we were seeing a lot of emphasis put on by regulatory agencies.
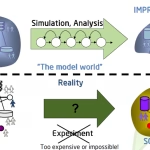
Modelling and simulation data can be highly supportive to avoid conducting additional clinical trials. Modelling can also be used assess the drug-drug interactions or potential overlapping toxicities, particularly in combination therapy, and effects of intrinsic and extrinsic factors, such as ethnicity, age, weight, renal and hepatic function. These factors can all have effects on how patient responds to the treatment.
When all the data is combined, the FDA has allowed for a new meeting, called a Type D meeting, which allows for a targeted discussion on RP2D and the supporting information. We can review if the available data you have is sufficient, to increase the likelihood the regulatory agency will agree with the recommended Phase 2 dose (RP2D) and be allowed to proceed on to the Phase 2 study.
We can also advise on the minimum number of doses required to explore in expansion and the number of patients in each dose level. Additionally, we can help review and compile all the available clinical data and any supporting non-clinical data to help justify and gain acceptance of the RP2D ahead of any large pivotal or confirmatory studies.
What is the ideal trial design for identifying the optimal dose?
It will depend a lot multiple factors such as the drug type, the indication, as well as operational and enrolment constraints in a particular patient population. In general, we have seen a shift from away from the traditional 3+3 design, which has been around now for nearly 80 years to new model shifted study design, such as the Bayesian optimised interval or BOIN design, which received regulatory acceptance as a fit for purpose design methodology in 2021.
These model assisted designs have shown a better ability to select the true maximum tolerated dose or optimum biologic dose, and typically will treat less patients at both inefficacious doses, as well as less patients at overly toxic doses, while still being similarly easy to understand and implement as that traditional 3+3 design.
Overall, the best protocol design is likely the one that causes the least delays while still providing the opportunity for informed decisions.
Final thoughts on overcoming challenges of Project Optimist and avoiding clinical hold.
Overall, the sponsor needs to maximise the knowledge from pharmacology and non-clinical exposure data, leverage any clinical pharmacodynamic biomarkers, and if available, continuous endpoints are most useful.
The FDA really tries to provide opportunities to help sponsors. We recommend that sponsors engage with the FDA at the appropriate time. Take advantage of the pre-IND meetings and the end of Phase 1 meeting with the new Type D meetings. Targeted questions can be asked and can have a shorter turnaround time compared to the other meeting types that the agency provide. Be aware of your accumulating clinical data as it would match to the non-clinical data that justifies from your product attribute, and then finally work with a CRO experience in clinical trial methods, particularly within a translational research phase.

